Let’s talk about your cycle so that there’s a greater understanding of what’s going on here.
A normal menstrual cycle is usually 28 +/- 7 days, in length (yes, many stray outside of this range). (1)
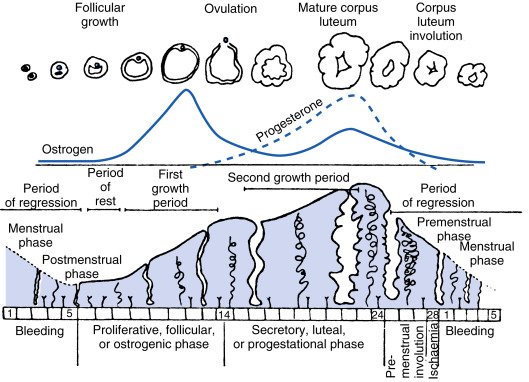
You have two phases to your cycle: your follicular phase and luteal phase.
In the first (follicular) phase, your estrogen levels will increase as the body prepares for ovulation (releasing an egg).
The second (luteal) phase starts with ovulation, and progesterone will then increase.
If the egg doesn’t become fertilized by sperm (and therefore, there is no pregnancy), both estrogen and progesterone will decrease and you’ll eventually get your period. The first day of your cycle is the first day of heavy menstrual bleeding.
Figure 4.25 from Shaw ST, Roche PC. Menstruation. In: Finn CA, ed. Oxford Review of Reproductive Endocrinology. vol 2. London: Oxford University Press; 1980.
There is way more depth to this cycle, but for the sake of this topic, we’ll keep it at that so you have a better understanding of what the luteal phase is. As Naturopathic Doctors, we’ll inquire about the length of your period, its flow, consistency, clotting, and PMS symptoms associated with your cycle.
So, to summarize and simplify – the follicular phase starts with the onset of your period. The luteal phase is the period between ovulation and the start of your period. It’s a cycle between the two phases. The follicular phase (first phase) tends to be more variable in it’s length (in days), whereas the luteal phase is often more consistent. These phases also change in length and characteristic with age, as the luteal phase tends to decrease from 14 days to 10 days in women who are over 40 years old. (1)
Okay, so - if you’re a woman, you’ve likely experienced premenstrual syndrome (PMS) symptoms. For the most part, majority of women I know & work with deal with PMS.
If you’re a woman and have experienced a number of cycles, it’s probably pretty easy to figure out that you’ll deal with those PMS symptoms in the second half, the luteal phase.
Premenstrual syndrome (PMS) is technically defined as a recurring group of mild-moderate symptoms (both physical and behavioural), which occur in the second half (luteal phase) of the menstrual cycle. These changes can interfere with normal daily activities and negatively affect interpersonal relationships – fair enough, no? These PMS symptoms are then followed by a period of time where they have essentially resolved themselves (at least temporarily) – usually resolving within a few days of menstruation (bleeding).
The most common physical complaints of PMS include: bloating, breast tenderness and headaches. Fatigue, changes in appetite (overeating, specific food cravings), insomnia or excessive sleeping, and muscle pain are a few other symptoms worth mentioning. (2)
The most common behavioural complaints of PMS include: depression, anxiety and irritability. There’s usually ‘marked affective lability,’ meaning that there’s a heightened sensitivity and reaction to events that might not usually cause such significant reactions. (2) And let’s be honest with ourselves – I’ve been able to figure out that my period is due just by checking in with my emotional state. Crying over a butter commercial is a pretty decent sign that I’m due.
That being said, more than 150 symptoms have been linked to PMS – so, this list is definitely not extensive.
Now, there’s something called Premenstrual Dysphoric Disorder (PMDD) which is actually considered a mental health diagnosis (found in the DSM). Essentially, this is a more severe form of PMS with significantly disabling symptoms – many of which are associated with emotional changes.
The DSM-V requires the presence of a number of diagnostic criteria (including a few of those PMS symptoms I’ve already mentioned) to be present for MOST menstrual cycles within the past year. Those symptoms are usually present during the last week of that luteal phase, with remission beginning within a few days after the follicular phase has started (once your period has started) and is absent during the week after menses. With PMDD, these physical and behavioural disturbances greatly interfere with the ability to function at work and/or school, being able to engage in basic social activities and start to impede on interpersonal relationships. Now all that said, PMDD is not just a ‘heightened’ state or exacerbation of major depressive disorder, panic disorder, personality disorder, a medication or another medical condition (ex. hyperthyroidism) – it is a whole matter in itself, and could in fact, be superimposed on top of one of those disorders. Some of those other affective disorders may actually be worse in the luteal phase but are not symptom-free in the mid-follicular phase (days 6-10), the way PMS (or PMDD) would often present. (2)
The most useful tool in monitoring PMS and PMDD is a prospective symptom diary. We get patients to do monthly tracking (across the entire cycle) to greater understand the severity of problems and determine any progress made with treatment.
Typical treatment of PMDD may involve an antidepressant (usually a serotonin reuptake inhibitor [SSRI]), oral contraceptives and may include other medications that target symptoms like bloating and breast pain. (2)
So, what are some interventions that Naturopathic Doctors (NDs) might consider?
Dietary interventions: the use of cruciferous vegetables, potentially removing dairy and/or caffeine from the diet, adding in natural, safe sources of phytoestrogens, assessing calcium intake (3,4), and ensuring proper proteins and essential fatty acids.
Physical activity recommendations.
Vitamin B6 (5,6)
Magnesium (7)
Ginger (8)
Botanical medicines: Chasteberry (Vitex agnus-castus) (5,9)
Recommendations for Cognitive Behavioural Therapy (CBT) (10) and yoga (11)
As always, do not Dr. Google yourself and self-prescribe these interventions. Always speak to a healthcare provider before starting anything new. Natural health products and botanical medicines can interact with medications/supplements, are not always indicated when it comes to particular health conditions, and should always be looked into by a professional.
If you’re looking to regulate your cycle, sort out symptoms of your cycle or gain a better understanding of your cycle, book an appointment with Sam here.
Reference(s):
(1) Douglas, N. Lobo, R. Comprehensive Gynecology: Reproductive Endocrinology: Neuroendocrinology, Gonadotropins, Sex Steroids, Prostaglandins, Ovulation, Menstruation, Hormone Assay. 4, p. 77-107. E1.
(2) Mendiratta, V. Lentz, G. Comprehensive Gynecology: Primary and Secondary Dysmenorrhea, Premenstrual Syndrome, and Premenstrual Dysphoric Disorder: Etiology, Diagnosis, Management. 37, p. 815-828. E3.
(3) PMID: 28217679
(4) PMID: 29560810
(5) PMID: 19923637
(6) PMID: 10334745
(7) PMID: 28392498
(8) PMID: 24944825
(9) PMID: 11159568
(10) PMID: 19247573
(11) PMID: 30712751